
They may nap during normal activities such as eating and talking.Patients with narcolepsy have persistent sleepiness, which may be irresistible.EDS and cataplexy are the key diagnostic symptoms.
However, many patients do not have all these features. There is a tetrad of classic narcolepsy symptoms: excessive daytime sleepiness (EDS), cataplexy, hypnagogic hallucinations and sleep paralysis. Cataplexy, sleep paralysis and hypnagogic hallucinations may be due to REM sleep intruding into wakefulness.

Narcolepsy is associated with a specific HLA allele, DQB1*0602.Possibly, immunological mechanisms may lead to loss of hypocretin. Narcolepsy may be caused by the loss of a relatively few neurons that are responsible for producing the neuropeptide hypocretin in the CNS. This is derived from the hypothalamus and is thought to be involved in sleep/wake cycles, food intake and pleasure-seeking behaviour. The peptide hypocretin (orexin) may be involved.The precise cause of narcolepsy is unknown both environmental and genetic factors may play a part: First-degree relatives are at increased risk of narcolepsy compared with the general population.
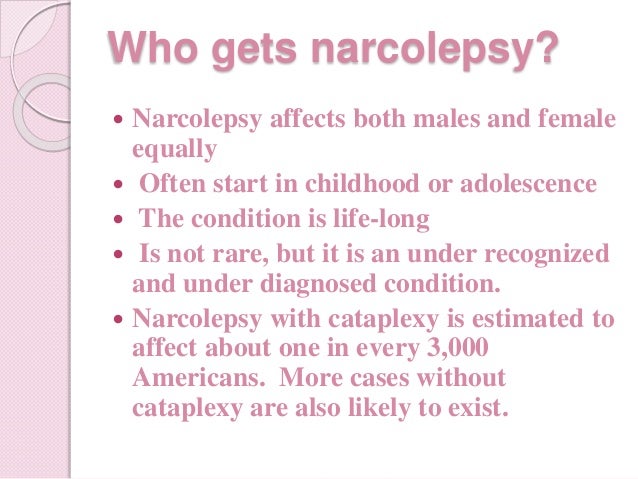
It is possible that incidence statistics would increase if diagnostic features were recognised at an earlier age. One study found that narcolepsy with cataplexy was often linked to complex movement disorders. Less than 5% of narcolepsy with cataplexy occurs in children.A smaller number of narcolepsy cases presents at around 35 years. Age of onset is typically around adolescence.P atients with narcolepsy without cataplexy are thought to represent only 36% of all narcolepsy patients. The prevalence of narcolepsy type 1 is between 25 and 100 per 100,000 people.


 0 kommentar(er)
0 kommentar(er)
